Drug-Free Strategies to Lower Your Blood Pressure
November 30, 2016 | 103,908 views
Google Tag Manager End Google Tag Manager
By Dr. Mercola
According to the Centers for Disease Control and Prevention (CDC), 1 in 3 American adults (about 70 million people) have high blood pressure.1 About half have uncontrolled high blood pressure, which increases your risk for a number of serious health problems, including:
- Heart disease
- Stroke
- Kidney disease2
- Cognitive decline, dementia and Alzheimer's disease3,4
Globally, more than 1 billion people struggle with high blood pressure, and prevalence has nearly doubled in the past four decades.5,6
Overall, men tend to have higher blood pressure than women, and while high-income nations have seen a significant decline in hypertension, prevalence in low- and middle-income countries, such as South Asia and Africa, is spiking. According to researchers, prevalence is "completely inverse" to national income.
Worldwide, high blood pressure is thought to cause nearly 13 percent of all deaths, or about 7.5 million deaths annually.
What Causes High Blood Pressure?
According to medical physiology textbooks, as much as 95 percent of hypertension is called essential hypertension, meaning the underlying cause is unknown. From my perspective, this simply isn't true. A number of factors have been identified as contributing to high blood pressure, including but not limited to:
• Insulin and leptin resistance. As your insulin and leptin levels rise, it causes your blood pressure to increase7,8
• Elevated uric acid levels are also significantly associated with hypertension, so any program adopted to address high blood pressure needs to normalize your uric acid level as well
• Poor nutrition in childhood has been shown to raise the risk of high blood pressure in adulthood9
• Lead exposure
• Pollution. As your insulin and leptin levels rise, it causes your blood pressure to increase
• Insulin and leptin resistance. Air pollution affects blood pressure by causing inflammation while noise pollution asserts an effect via your nervous and hormonal systems.
Air pollution has been shown to increase your risk of high blood pressure to the same degree as having a body mass index (BMI) of 25 to 30.
Living in an area plagued by constant noise pollution (busy city streets with night time traffic) has been shown to increase the risk of hypertension by 6 percent, compared to living in an area where noise levels are at least 20 percent lower10
The Importance of Diet and Insulin Sensitivity
As noted by the lead author Majid Ezzati, Ph.D., a professor of global environmental health at Imperial College London:11
"The perception is that people are not getting enough calories, but the reality is, they're not getting healthy calories. Making fresh, healthy food affordable and accessible for everybody should be a priority."
One of the most important dietary changes needed to improve high blood pressure is to eliminate or dramatically reduce sugar and processed fructose from your diet. The easiest way to do that is to replace processed foods with real, whole foods. This will address not only insulin and leptin resistance but also elevated uric acid levels.
One 2010 study12 discovered that those who consumed 74 grams or more per day of fructose (the equivalent of about 2.5 sugary drinks) had a 77 percent greater risk of having blood pressure levels of 160/100 mmHg (stage 2 hypertension).
Consuming 74 grams or more of fructose per day also increased the risk of a 135/85 blood pressure reading by 26 percent, and a reading of 140/90 by 30 percent. To learn more about healthy eating, please see my optimal nutrition plan, which will guide you through the necessary changes step-by-step.
To ascertain whether insulin/leptin resistance is at play, be sure to check your fasting insulin level. If your hypertension is the result of elevated insulin levels, dietary intervention will be key.
Aim for a fasting insulin level of 2 to 3 microU per mL (mcU/mL). If it's 5 mcU/mL or above, you definitely need to lower your insulin level to reduce your risk of high blood pressure and other cardiovascular health problems.
Keep in mind that the so-called "normal" fasting insulin level is anywhere from 5 to 25 mcU/mL, but please do not make the mistake of thinking that this "normal" insulin range equates to optimal.
Do You Have High Blood Pressure?
A blood pressure reading gives you two numbers. The upper or first number is your systolic blood pressure reading. The lower or second number is your diastolic pressure. For example, a blood pressure reading of 120 over 80 (120/80) means you have a systolic arterial pressure of 120 and a diastolic arterial pressure of 80.
Your systolic pressure is the highest pressure in your arteries. It occurs when your ventricles contract at the beginning of your cardiac cycle. Diastolic pressure refers to the lowest arterial pressure, and occurs during the resting phase of your cardiac cycle. Ideally, your blood pressure should be about 120/80 without medication.
If you're over the age of 60, your systolic pressure is the most important cardiovascular risk factor. If you're under 60 and have no other major risk factors for cardiovascular disease, your diastolic pressure is believed to be a more important risk factor.13
According to guidelines14,15,16 issued by the Joint National Committee (JNC) on Prevention, Detection, Evaluation and Treatment of High Blood Pressure in 2014, the following blood pressure classifications are used to determine whether you might suffer from hypertension:17
Blood Pressure Classification
|
Systolic Pressure (mmHg)
|
Diastolic Pressure (mmHg)
|
Normal
|
<120 span="">
|
<80 span="">
|
Pre-hypertension
|
120-139
|
80-89
|
Stage 1 Hypertension
|
140-159
|
90-99
|
Stage 2 Hypertension
|
≥160
|
≥100
|
How to Avoid a False Hypertension Diagnosis
To avoid a false hypertension diagnosis, keep in mind that your blood pressure reading can vary significantly from day to day, and even from one hour to the next, so don't overreact if you get one high reading here or there. It's when your blood pressure remains consistently or chronically elevated that significant health problems can occur. The following variables can also affect the validity of your blood pressure reading:
• Incorrect blood pressure cuff size: If you're overweight, taking your reading with a size "average" blood pressure cuff can lead to a falsely elevated blood pressure reading, so make sure your doctor or health care professional is using the right size cuff for your arm.
• Incorrect arm position: If your blood pressure is taken while your arm is parallel to your body, your reading can be up to 10 percent higher than it really is. Blood pressure readings should always be taken with your arm at a right angle to your body.
• Nervousness: "White coat hypertension" is a term used for when a high blood pressure reading is caused by the stress or fear associated with a doctor or hospital visit. This can be a transient yet serious concern. If this applies to you, stress reduction is key.
To decrease your risk of being falsely diagnosed with hypertension in this situation, take a moment to calm down (be sure to arrive for your appointment ahead of time so you can unwind), then breathe deeply and relax when you're getting your blood pressure taken.
Measuring Pressure on Both Arms May Provide Valuable Health Info
More recently, researchers are urging healthcare providers to measure blood pressure twice, once on each arm. A number of studies have revealed that a significant difference between your right and left arm pressure may indicate circulatory problems that raise your risk for stroke, peripheral artery disease or other cardiovascular problems.18
Slight variations in blood pressure between left and right is normal, but when the difference is five points or greater, it could signal trouble. A British study found that people with a five-point or more difference between arms had nearly double the risk of dying from heart disease in the next eight years.19
Another analysis of 20 studies found that those with a right-to-left arm difference in blood pressure of 15 points or more were twice as likely to have peripheral artery disease in the arms and/or legs. As noted by Harvard Health Publications:20
"In younger people, side-to-side differences in blood pressure can occur when a muscle or something else compresses an artery supplying the arm, or by a structural problem that prevents smooth blood flow through an artery. In older people, it's usually due to a blockage arising from atherosclerosis, the artery-clogging disease process at the root of most heart attacks, strokes, peripheral artery disease and other cardiovascular conditions.
A less common cause of a between-arm difference in blood pressure is an aortic dissection. This is a tear inside the wall of the aorta, the main pipeline of oxygenated blood from the heart to the body. At your next doctor's visit, ask to have your blood pressure checked in both arms. If there's a difference greater than 10 point, another test called the ankle-brachial index might be in order to check for peripheral artery disease."
Treatment Recommendations
If you're between the ages of 18 and 59 without major health conditions, or if you're 60 or older with diabetes and/or chronic kidney disease, conventional medicine recommends drug treatment if your blood pressure is at or above 140/90. In those over 60 who do not have diabetes or chronic kidney disease, the panel suggests delaying drug treatment until you're above 150/90. According to the JNC panel members:21
"For all persons with hypertension, the potential benefits of a healthy diet, weight control and regular exercise cannot be overemphasized. These lifestyle treatments have the potential to improve BP control and even reduce medication needs. Although the authors of this hypertension guideline did not conduct an evidence review of lifestyle treatments in patients taking and not taking antihypertensive medication, we support the recommendations of the 2013 Lifestyle Work Group."22
While recommending diet and exercise is a step in the right direction, the panel didn't take it all the way. In my experience, even stage 1 and 2 hypertension can be successfully addressed with lifestyle interventions, to where drugs become unnecessary.
The key is to be sufficiently aggressive in your diet and lifestyle modifications. There are plenty of clinical success stories that vouch for this stance.23 That said, if you have seriously elevated blood pressure, it would be wise to be on medication to prevent a stroke while you implement these lifestyle changes.
Omega-3 Is Vital for Healthy Blood Pressure
Recent research highlights the importance of animal-based omega-3 fats for healthy blood pressure — especially in young adults. More than 2,000 healthy men and women between the ages of 25 and 41 participated in the study. Diabetics and those with a BMI over 35, which is considered obese, were excluded.
The findings showed that those with the highest serum levels of omega-3 also had the lowest blood pressure readings. On average, their systolic pressure was 4 millimeters of mercury (mm Hg) lower and their diastolic pressure was 2 mm Hg lower compared to those with the lowest omega-3 blood levels. As reported by WebMD:24
"'This suggests that promoting diets rich in omega-3 foods could be a strategy to prevent high blood pressure,' [Dr. Mark] Filipovic said … Even a small reduction in pressure, as little as about 5 mm Hg, could prevent a great number of strokes and heart events in the general population …
Another recent study found that doses of omega-3 fatty acids as low as less than a gram a day could help those who already have high blood pressure reduce their numbers … The fish oil may work by improving blood vessel function and reducing inflammation, among other things,' Filipovic said."
Animal-Based Versus Plant-Based Omega-3s
An error occurred.
You can obtain omega-3 fats from both plants and marine animals like fish and krill. However, it's really important to realize that these sources provide very different types of omega-3 and, as explained by Nils Hoem, Ph.D., a Norwegian scientist specializing in omega-3 phospholipids, they are NOT interchangeable.
The short-chain fatty acids found in plants are simply food — they're a source of energy — while the long-chain fatty acids found in fish and krill, especially docosahexaenoic acid (DHA), are structural elements that actually make up your cells. This is a MAJOR difference between plant- and animal-based sources.
There are specific transporters for long-chained omega-3s in your blood-brain barrier, the placenta (in pregnant women), and likely also in your liver, which transport these molecules in a very precise way into the cell membranes where they belong. No such transporters exist for the short-chained omega-3s.
So please, don't make the mistake of confusing plant-based (short-chained) and animal-based (long-chained) omega-3, as doing so could have severe health consequences. You absolutely need animal-based omega-3, and you simply cannot obtain the same benefits from plant-based sources because the conversion rate of plant-based ALA omega 3 fats to DHA is clinically insignificant.
Fish and krill also have differences worth noting. One of the most important differences is the fact that krill oil is bound to phospholipids, which allows the omega-3 fats to travel efficiently into your hepatic system; hence, they're more bioavailable. Phospholipids are also a principal compound in high-density lipoproteins (HDL), which you want more of, and by allowing your cells to maintain structural integrity, phospholipids help your cells function properly.
Finally, many vegans are using marine-based DHA supplements, which makes sense but is still less than ideal, as you not only need DHA but the whole complex of supporting fatting acids. Do your best to get your DHA from healthy, nontoxic seafood, and if that is not possible, then use a high-quality full spectrum DHA supplement like krill oil.
You can learn more about all of these differences by listening to the interview above, or reading through the accompanying article," The Critical Differences Between Omega-3 Fats From Plants and Marine Animals." A summary can also be found in the following infographic.
Embed this infographic on your website:
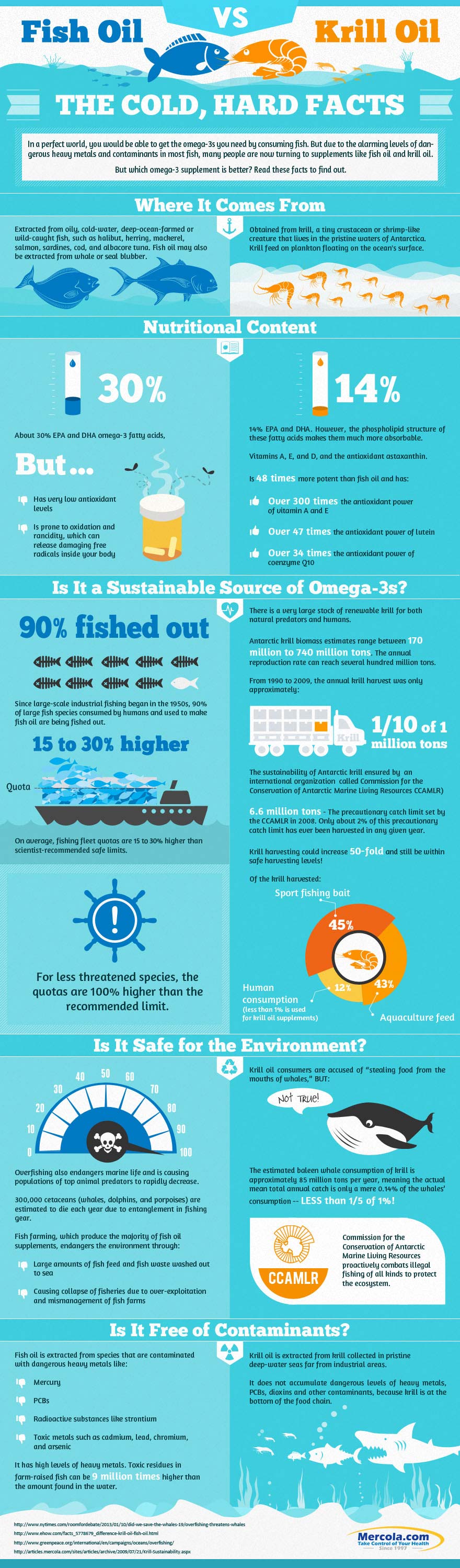
Learn why krill oil is a safer and smarter choice than fish oil through the Fish Oil versus Krill Oil: The Cold, Hard Facts infographic. Use the embed code to share it on your website or visit our infographic page for the high-res version.
<img src="http://media.mercola.com/assets/images/infographic/krill-oil-vs-fish-oil.jpg" alt="krill oil vs fish oil infographics" border="0" style="max-width:100%; min-width:300px; margin: 0 auto 20px auto; display:block;"><p style="max-width:800px; min-width:300px; margin:0 auto; text-align:center;">Learn why krill oil is a safer and smarter choice than fish oil through the <a href="http://www.mercola.com/infographics/fish-oil-vs-krill-oil.htm"><strong>Fish Oil versus Krill Oil: The Cold, Hard Facts</strong></a> infographic. Visit our infographic page for the high-res version.</p>
Click on the code area and press CTRL + C (for Windows) / CMD + C (for Macintosh) to copy the code
Beetroot Juice May Help Lower Blood Pressure
Another food that has been found to have a beneficial effect on blood pressure is beetroot juice.25 In one small placebo-controlled trial, one glass (250 milliliters or 8.5 ounces) of beetroot juice per day for one month reduced blood pressure in those diagnosed with hypertension by an average of 8 mmHg systolic and 4 mmHg diastolic pressure.26
This 8/4 mmHg reduction is very close to that provided by blood pressure mediations, which typically can reduce blood pressure by about 9/5 mmHg, and for many it was enough to bring their blood pressure down to normal levels. The treatment group also saw a 20 percent improvement in blood vessel dilation capacity and a 10 percent reduction in arterial stiffness.
However, within two weeks of stopping the juice, their blood pressure returned to their previous levels, so you'd have to keep drinking it consistently. For this reason, I would advise against viewing beetroot juice as a primary solution. A better strategy would be to incorporate a glass of beetroot juice as a short-term solution while you're implementing other dietary changes and exercise.
The beneficial effects are related to the nitrate (NO3) found in beetroot juice. Your body converts the NO3 into bioactive nitrite (NO2) and nitric oxide (NO), the latter of which helps relax and dilate your blood vessels, and helps prevent blood clots. Other vegetables high in NO3 include:
Radishes
|
Kale
|
Celery
|
Mustard greens
|
Turnip tops
|
Spinach
|
Cabbage
|
Eggplant
|
Leeks
|
Scallions
|
String beans
|
Carrots
|
Garlic Is Also Helpful
Two other foods known to dilate blood vessels, albeit in different ways from beetroot juice, are garlic and watermelon. In an experiment by the British BBC series, "Trust Me, I'm a Doctor," designed to evaluate which of these three foods was the most effective for lowering blood pressure, found that beetroot produced the greatest results.
It lowered blood pressure of the 28 participants from an average baseline of 133.6 mmHg to 128.7 mmHg in one week. Garlic came in second place, lowering blood pressure to an average of 129.3 mmHg. Watermelon, in last place, lowered blood pressure to an average of 129.8 mmHg. As noted by BBC:27
"Our small study adds to a growing number which suggest that eating beetroot and garlic regularly may help reduce your blood pressure. But these aren't the only foods that can do this. The active ingredient in beetroot, nitrate, is present in plenty of green vegetables: celery; lettuce; watercress; rocket; spinach; chard; broccoli; for example.
And the active ingredient in garlic — allicin — is also present in onions, shallots, leeks, chives and spring onions. It turns out there are several foods which can help keep our blood pressure low."
Vitamin D Can Also Relax Your Arteries and Improve Blood Pressure
Vitamin D deficiency, associated with both arterial stiffness and hypertension,28 is another important consideration. According to researchers from the Emory/Georgia Tech Predictive Health Institute,29 even if you're considered generally "healthy," if you're deficient in vitamin D then your arteries are likely stiffer than they should be. As a result, your blood pressure may run high due to your blood vessels being unable to relax.
In their study, having a serum level of vitamin D lower than 20 nanograms per milliliter (ng/ml) was considered a deficiency state that raises your hypertension risk. Less than 30 ng/ml was deemed insufficient. Previous research30 has also shown that the farther you live from the equator, the higher your risk of developing high blood pressure.
Blood pressure also tends to be higher in winter months than during the summer. Exposing your bare skin to sunlight affects your blood pressure through a variety of different mechanisms, including the following:
• Sun exposure causes your body to produce vitamin D. Lack of sunlight reduces your vitamin D stores and increases parathyroid hormone production, which increases blood pressure.
• Vitamin D deficiency has also been linked to insulin resistance and metabolic syndrome, a group of health problems that can include insulin resistance, elevated cholesterol and triglyceride levels, obesity and high blood pressure.
• Research31 shows that sun exposure increases the level of NO in your skin. This dilates your blood vessels, thereby reducing your blood pressure. (For comparison, and to show how various factors tie together, uric acid, produced when you eat sugar/fructose, raises your blood pressure by inhibiting NO in your blood vessels — the opposite effect of sun exposure.)
• Vitamin D is also a negative inhibitor of your body's renin-angiotensin system (RAS), which regulates blood pressure.32 If you're vitamin D deficient, it can cause inappropriate activation of your RAS, which may lead to hypertension.
• Exposure to ultraviolet (UV) rays is thought to cause the release of endorphins, chemicals in your brain that produce feelings of euphoria and relief from pain. Endorphins naturally relieve stress, and stress management is an important factor in resolving hypertension.
Key Lifestyle Strategies for Lowering Your Blood Pressure
In summary, here are several suggestions that can help lower your blood pressure naturally.
Address insulin and leptin resistance
As mentioned earlier, high blood pressure is typically associated with insulin resistance, which results from eating a diet too high in sugar. As your insulin level elevates, so does your blood pressure. Insulin stores magnesium, but if your insulin receptors are blunted and your cells grow resistant to insulin, you can't store magnesium so it passes out of your body through urination.
Magnesium stored in your cells relaxes muscles. If your magnesium level is too low, your blood vessels will constrict rather than relax, and this constriction raises your blood pressure.
Fructose also elevates uric acid, which drives up your blood pressure by inhibiting the NO in your blood vessels. (Uric acid is a byproduct of fructose metabolism. In fact, fructose typically generates uric acid within minutes of ingestion.) NO helps your vessels maintain their elasticity, so NO suppression leads to increases in blood pressure.
If you're healthy, and want to stay that way, the general rule is to keep your total fructose intake to 25 grams per day or less. If you're insulin resistant and/or have high blood pressure, keep your total fructose to 15 grams or less per day until your condition has resolved.
|
Eat real food
A processed food diet, loaded with net carbohydrates (non-fiber carbs like sugar, fructose and grains) and trans fat (margarines and vegetable oils) is a recipe for hypertension. Instead, make whole, ideally organic foods the focus of your diet.
Also remember to swap non-fiber carbs for healthy fats such as avocados, butter made from raw, grass-fed organic milk, organic pastured egg yolks, coconuts and coconut oil, raw nuts such as pecans and macadamia, grass-fed meats and pasture raised poultry. To learn more about healthy eating, please see my optimal nutrition plan.
|
Mind your sodium to potassium ratio
According to Lawrence Appel, lead researcher on the DASH diet and director of the Welch Center for Prevention, Epidemiology and Clinical Research at Johns Hopkins, your diet as a whole is the key to controlling hypertension — not salt reduction alone.
He believes a major part of the equation is this balance of minerals — i.e., most people need less sodium and more potassium, calcium and magnesium. According to Appel:33 "Higher levels of potassium blunt the effects of sodium. If you can't reduce or won't reduce sodium, adding potassium may help. But doing both is better."
Indeed, maintaining a proper potassium to sodium ratio in your diet is very important, and hypertension is but one of many side effects of an imbalance. A processed food diet virtually guarantees you'll have a lopsided ratio of too much sodium to potassium. Making the switch from processed foods to whole foods will automatically improve your ratios.
|
Load up on veggies
Juicing is a simple way to increase the amount of vegetables in your diet, and many NO3-rich veggies (which raise your NO level) are suitable for juicing, such as beets, kale, celery, spinach, carrots and more. Allicin-rich garlic, leeks, challots and chives also help improve your blood pressure, and are easy to add to salads and various dishes.
|
Optimize your vitamin D level
To learn more about vitamin D testing, please see my previous article, "How Vitamin D Performance Testing Can Help You Optimize Your Health."
|
Boost your animal-based omega-3 intake
The best way to boost your omega-3 is to eat plenty of oily fish that are low in mercury and other pollutants. Good options include wild caught Alaskan salmon, sardines and anchovies. Alternatively, take a high-quality krill oil or fish oil supplement. As noted earlier, krill oil has certain advantages over fish oil, which is why I prefer it.
|
Consider intermittent fasting
Intermittent fasting is one of the most effective ways I've found to normalize your insulin/leptin sensitivity. It's not a diet in conventional terms, but rather a way of scheduling your eating in such a way as to promote efficient energy use.
Essentially, intermittent fasting means eating your calories during a specific window of the day, and choosing not to eat food during the rest. When you eat, your body reacts by elevating insulin and leptin.
|
Exercise regularly
A comprehensive fitness program can go a long way toward regaining your insulin sensitivity and normalizing your blood pressure. To reap the greatest rewards, I recommend including high intensity interval exercises in your routine.
If you are insulin resistant, you'll also want to include weight training. When you work individual muscle groups, you increase blood flow to those muscles, and good blood flow will increase your insulin sensitivity.
I also recommend training yourself to breathe through your nose when exercising, as mouth breathing during exercise can raise your heart rate and blood pressure, sometimes resulting in fatigue and dizziness. To learn more about this, please refer to my previous article on the Buteyko breathing method.
|
Avoid smoking and other forms of pollution
Smoking is known to contribute to high blood pressure, as are other forms of air pollution, and even noise pollution. To address these, avoid smoking, consider using ear plugs during sleep if you live in a noisy neighborhood (provided you cannot move), and take steps to improve your indoor air quality.
|
Walk barefoot
Going barefoot will help you ground to the earth. Experiments show that walking barefoot outside (also referred to as Earthing or grounding) improves blood viscosity and blood flow, which help regulate blood pressure.So, do yourself a favor and ditch your shoes now and then.
Grounding also calms your sympathetic nervous system, which supports your heart rate variability. This in turn promotes homeostatis, or balance, in your autonomic nervous system. In essence, anytime you improve heart rate variability, you're improving your entire body and all of its functions.
|
Address your stress
The connection between stress and hypertension is well documented, yet still does not receive the emphasis it deserves. In fact, it has been shown that people with heart disease can lower their risk of subsequent cardiac events by over 70 percent simply by learning to manage their stress.
Suppressed negative emotions such as fear, anger and sadness can severely limit your ability to cope with the unavoidable every day stresses of life. It's not the stressful events themselves that are harmful, but your lack of ability to cope.
The good news is, strategies exist to quickly and effectively transform your suppressed, negative emotions, and relieve stress. My preferred method is the Emotional Freedom Techniques (EFT), an easy to learn, easy to use technique for releasing negative emotions.
EFT combines visualization with calm, relaxed breathing, while employing gentle tapping to "reprogram" deeply seated emotional patterns.
|
1 comment:
3 Studies REVEAL How Coconut Oil Kills Fat.
The meaning of this is that you actually burn fat by consuming Coconut Fat (including coconut milk, coconut cream and coconut oil).
These 3 researches from big medical journals are sure to turn the conventional nutrition world around!
Post a Comment